Surgery
In some cases, surgery may be recommended to alleviate symptoms or slow the progression of mesothelioma. Surgery may be performed in tandem with other treatments such as chemotherapy and radiation, also known as “multi-modal therapy.”
As scientists develop tests to diagnose mesothelioma at an earlier stage, surgery could play a role in curing the disease in the future. Doctors specializing in mesothelioma are working toward the goal of using surgery to remove the cancer and the necessary surrounding tissue in an effort to stabilize the disease.
Whether a surgery is recommended for a particular patient will depend on factors unique to each person, including the type and location of the cancer, the “stage” of the cancer and the patient’s overall health.
Even among the subgroup of patients for whom surgery is an appropriate option, there are a variety of surgical procedures that may be considered—some to control the buildup of fluid that can cause such discomfort and others to remove the tumor mass and slow progression of the disease.
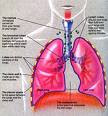
For a patient with pleural mesothelioma, which affects the membrane surrounding the lungs, a surgeon may be called up to perform a thoracentesis, pleurodesis or pleurectomy/decortication to relieve or control discomfort and plural effusion, the buildup of fluid around the lungs that can cause pain and shortness of breath. Other surgeries, such as a pneumonectomy or an extrapleural pneumonectomy, remove more extensive tissue in an attempt to slow tumor progression.
For a patient dealing with peritoneal mesothelioma, which attacks the membrane lining the abdomen, the surgeon may relieve a peritoneal effusion, the buildup of fluid in the abdomen, through a paracentesis. The lining of the abdomen, called the peritoneum, may be removed by a peritonectomy. In a cytoreductive surgery, surgeon will open the abdomen and remove every visible sign of cancer.
Finally, for patients dealing with the most rare form of mesothelioma that involves the membrane surrounding the heart (pericardial mesothelioma), a surgeon might perform a pericardiocentesis to drain the buildup of fluid around the heart, or the more aggressive extrapleural pneumonectomy may be used in some cases to remove the tumor and surrounding tissues.
Types of surgery for mesothelioma treatment:
Thoracentesis
This procedure involves the draining of fluid that may build up (called a “pleural effusion”) in the chest between the lung and the pleura. A tube is placed in the chest in order to drain out the fluid. Thoracentesis is a palliative treatment, meaning that its purpose is to help relieve discomfort.
Pleurodesis
Pleurodesis is a surgical procedure to help control pleural effusion, which is the buildup of fluid between the lungs and the lung lining. Pleurodesis closes the space between the lung and the lung lining, reducing the chance for fluid to accumulate.
There are two approaches to performing a pleurodesis. In the first, a tube that is inserted into the chest drains the excess fluid. After this fluid is drained, a schlerosing agent (a substance that causes tissue to scar or harden), such as sterile talc powder, is injected through the chest tube and into the pleural space. The schlerosing agent is allowed to distribute itself through the pleural space, with the patient being asked to move about in order to facilitate the distribution. Once the agent is distributed, suction is applied to the tube in the chest. Similar to collapsing a plastic bag, the suction brings the two pleural surfaces together, allowing them to “scar” together.
The second method of pleurodesis uses thoracoscopy, whereby a small incision, or a series of small incisions, are made in the skin. A thoracoscope is passed through the incision in order to get a better look at the pleura. The schlerosing agent is then applied to the area.
Pleurectomy/decortication
Pleurectomy/decortication involves removing the pleura, where most of the tumor is located. This procedure may help control pleural effusions (fluid buildup) and help to decrease the pain caused by the tumor. It is a palliative treatment, meaning that its goal is to help to lessen the discomfort caused by mesothelioma.
Pneumonectomy
A pneumonectomy is the removal of all or part of the lung. Your surgeon will make an incision in the side of the chest. When the lung is revealed, the surgeon visually assesses the tumor and decides how much tissue should be removed.
Extrapleural Pneumonectomy
This extensive surgery usually involves the removal of the pleura, pericardium, diaphragm and the whole lung on the side of the cancerous tumor. Your surgeon may decide to remove some of the surrounding tissues as well.
Paracentesis
Peritoneal mesothelioma can cause fluid to build up in the abdomen in a process called peritoneal effusion. This excess fluid is drained through a needle and tube inserted into the abdomen. Paracentesis (sometimes called an “ascitic tap”) can help take the pressure off the internal organs, and also helps reduce the risk of infection that may be caused by the fluid buildup. This is a “palliative” procedure, meaning that the goal of paracentesis is to help to relieve the discomfort associated with peritoneal mesothelioma.
Peritonectomy
A “peritonectomy” involves removing the peritoneum, the lining of the abdomen where the mesothelioma first develops. This form of surgery is most often used when the cancer is detected in the very early stages of the disease. Your surgeon might recommend that a peritonectomy be performed in tandem with “intraperitoneal hypothermic perfusion,” a form of heated chemotherapy where the chemotherapy drugs are administered directly into the abdomen during and/or after surgery.
Cytoreductive surgery
During cytoreductive or “debulking” surgery, the surgeon opens the abdominal cavity (a procedure known as a “laparotomy”) to look for all signs of cancer and attempt to remove as much of the tumor as possible. This surgery can be quite long in duration because of the amount of detail the surgeon must use to search for and remove signs of cancer in the abdominal area. Your surgeon might recommend that this surgery be performed in tandem with “intraperitoneal hypothermic perfusion,” a form of heated chemotherapy administered into the abdominal cavity.

Pericardiocentesis
This is the process for drawing fluid out of the affected area to help to relieve the discomfort associated with pericardial mesothelioma. For this procedure, a needle is inserted into the pericardium (the sac around the heart) to drain the fluid and relieve circulatory problems. The draining of this fluid can be associated with complications, however.
Radiation
Radiation therapy is an intense X-ray treatment to damage or kill cancer cells. Although not a cure for mesothelioma, radiation therapy nonetheless may be used at different stages of the disease to slow its growth. Radiation is often the main treatment for patients in weak health who are not candidates for surgery. When radiotherapy is used following surgical removal of the tumor, it is called adjuvant therapy. This type of therapy—surgery followed by radiation—has been demonstrated to reduce the local recurrence of the tumor and to improve the survival rate of patients with early-stage disease. Adjuvant therapy is also an essential part of the treatment of patients who undergo an extrapleural pneumonectomy.
Radiation therapy is important not just to control the growth of the tumor. Radiotherapy is also used to relieve the symptoms of mesothelioma by reducing pain, improving breathing, and easing the other physical problems caused by the cancer.
The kind of radiation treatment used for each patient will depend on several factors, including the size of the tumor and how close it is to vital organs, the stage of the disease, and whether other treatment options may also be used.
There are two primary types of radiation therapy used for mesothelioma patients: traditional external beam radiotherapy and brachytherapy. In addition, mesothelioma doctors are now employing a new form of radiotherapy, intensity-modulated radiation therapy (IMRT).
Adjuvant therapy
Adjuvant therapy is additional treatment to reduce the risk or cancer recurrence or increase the time before cancer recurs. Through the use of chemotherapy, radiation or other adjuvant therapies after a primary treatment like surgery, cancer specialists attempt to kill cancer cells that were left behind in the body but are too small to be seen. Adjuvant therapies, like all cancer treatments, also pose side effects that must be weighed in deciding whether to proceed with a possible treatment.

External Beam Radiation
External beam radiation therapy (EBRT) is routed to the site of the tumor with the use of linear accelerators. These machines generate high-energy external radiation beams that reach through the tissues into the areas where the tumor is found. To deliver the radiation precisely, doctors use computed tomography (CT) scans and PET scans to focus on the areas where the tumor is likely to reappear. Careful radiation planning allows the radiologist to direct a higher dose of radiation at the tumor tissue and to minimize the amount of normal tissue that will be exposed to this high dose of radiation.
Brachytherapy
Brachytherapy uses radioactive substances rather than radiation beams to deliver radiation treatments. The word “brachy” comes from the Greek, and means “short range.” This type of radiation therapy is different from external beam radiation, which is administered over a long range.
Because the radioactive substances used in brachytherapy will only work in the short range, they must be placed in or very near the target area of the body. This means that brachytherapy can be used for mesothelioma patients only by surgically implanting the radioactive substances. This therapy is generally performed during the same operation in which the tumor is removed, and is sometimes referred to as “Intraoperative Radiation Therapy” (IORT). For brachytherapy, the thoracic surgeon and radiation oncologist measure the areas of the chest cavity from which the mesothelioma and surrounding tissue cannot be fully removed. Then, a customized implant is created by weaving radioactive seeds into an absorbable mesh, known as a radioactive iodine seed implant. This flexible mesh is stitched into the body during surgery. The radiation from the implant is released over a three-month period, with a small amount of radioactivity still present for about a year. It is critical during this therapy not to increase a patient’s time in surgery too long, or complications may develop as a result of this delay. Doctors are still evaluating the overall benefits and risks of this procedure.
Intensity-modulated radiation therapy (IMRT)
Intensity-modulated radiation therapy (IMRT) is a new breakthrough in radiation oncology. The therapy allows for treatment of areas of the body that previously could not be treated with conventional radiation. IMRT for mesothelioma is delivered by a team of physicians, including a radiation oncologist, physicist and radiation therapist. The preliminary results for this new therapy suggest that the rate of local recurrence is significantly reduced for mesothelioma patients undergoing this treatment.
Chemotherapy
Chemotherapy uses certain chemical agents or drugs that are specifically destructive to malignant tissues and cells. Doctors may recommend single agent chemotherapy or a combination chemotherapy treatment. The single agent chemotherapy treatment involves the use of just one type of chemical or drug. The combination chemotherapy method involves the use of more than one chemical or drug. While it is not a cure for mesothelioma, chemotherapy treatment may help to prevent the spread of the disease or slow its growth. Chemotherapy may also shrink tumors before surgery is performed (called neoadjuvant therapy), destroy tumor cells still remaining after surgery (called adjuvant therapy), and relieve symptoms, such as pain (called palliative therapy).
Generally, chemotherapy drugs are delivered by injection into a vein. Depending on the type and location of the cancer and the drug used, however, the chemotherapy drugs may be delivered by mouth, into the muscle or skin or by placing the drugs directly into a body cavity (called intracavitary chemotherapy).
Chemotherapy drugs usually cause fatigue or exhaustion. Patients also may experience nausea, vomiting and hair loss. Specific side effects will vary, based on the drug, its dosage, and the length of treatment. Other chemotherapy-related drugs and therapies may minimize the side effects or will be prescribed for use following chemotherapy
Clinical Trials
Clinical trials are conducted on all new therapies and drugs before the FDA approves them for use by the general public. Many medications and treatments that are now the standard of care for certain diseases have gone through a lengthy period of testing with clinical trials. These carefully controlled studies are always in need of patients willing to try the experimental treatments. Many patients with aggressive illnesses or those with no known cure willingly participate in a clinical trial as a last hope. Patients should ask their doctors about currently available clinical trials to determine whether they might qualify to participate in a particular study. Those choosing to take part in a clinical trial should carefully weigh the risks and benefits before agreeing to participate.
.
A clinical trial has three stages. Phase I trials involve just a limited number of people. They generally focus on a drug’s correct dosage and relative safety. Phase II trials enlist more people and concentrate on whether the new drug is effective in fighting a particular illness. Phase III is the final phase of a clinical trial in which the new medication is compared against any existing treatment to determine whether the new treatment is more effective than the old.

Enrolling in a Clinical Trial
Many factors should be considered when deciding whether to take part in a clinical trial. Such trials usually are held in large metropolitan hospitals. Patients need to know how often they must see the physicians coordinating the trials and how much time each visit will take, since travel expenses can be quite costly.
Often, it is difficult to qualify for a clinical trial. To gain the most information possible from a clinical trial, the trial coordinator will place strict controls on the group of qualified patients. In some clinical trials, a patient must have already had unsuccessful traditional treatment. Other clinical trials only enroll patients who have not yet undergone any treatment for mesothelioma.
A patient’s general health will also affect qualification. Mesothelioma patients with other medical conditions and those taking drugs for other illnesses will likely be excluded from clinical trials. By studying only patients who are being treated for one disease with one therapy, researchers are given a more accurate assessment of the effectiveness of the experimental mesothelioma treatment.
Patients must also consider that participation in a clinical trial requires the relinquishment of control over medical treatment. For example, some clinical trials are referred to as randomized studies. In such trials, one group of patients receives the traditional treatment while another group is given the new experimental treatment. But the patients do not select which treatment they receive, nor are they told which treatment is being administered. A patient’s participation in a clinical trial is not a guarantee that the patient will receive anything other than the traditional therapy.
Still, there are enormous benefits associated with clinical trials. Without them, it would be very difficult to test the effectiveness of new medications. And clinical trials offer participants thorough and high quality health care. Meticulous records are kept and extensive testing is performed on each patient to gauge a new treatment’s effectiveness and safety. Clinical trials for mesothelioma are a critical part of finding a cure.
Ongoing Mesothelioma Clinical Trials
A variety of resources on the Internet discuss ongoing clinical trials for mesothelioma and include the qualifications for each trial. Patients interested in taking part in a clinical trial should consult their doctor. Physicians specializing in mesothelioma are kept abreast of all upcoming and current clinical trials, and are able to determine whether a patient qualifies for a particular trial. Large regional cancer centers also have access to current information on clinical trials that are coordinated through the regional hospitals.
Some of clinical trials are reportedly still recruiting participants; some are actively testing new treatments but are not currently seeking participants. Others have already been completed and may provide helpful information to physicians following the development of new mesothelioma treatments. More information about these trials and other clinical trials can be located on the Internet at the National Institute of Health’s Database of Clinical Trials, from which we have collected the information provided on this site. Again, patients should consult their doctors to determine whether a particular trial is available to them.
Innovative Mesothelioma Therapies
Traditional cancer treatment regimens such as radiation and chemotherapy are widely used for mesothelioma patients, but they do not offer a cure for the disease. Increasingly, patients have turned to unconventional forms of therapy in the hope that the answer lies with gene therapy, immunotherapy or photodynamic therapy. All of these treatment options should be discussed with the patient’s physician prior to setting out on a course of alternative treatment.
Gene Therapy
Gene therapy is a method for correcting defective genes that cause disease development. The therapy can work in several ways. Scientists can correct defective genes by removing, inserting, replacing, or altering genes in order to treat or prevent a disease.
To treat a disease such as mesothelioma, a carrier called a ‘vector’ would be used to deliver the therapeutic gene. Generally, viruses are used because they already have the capacity to invade a cell. Also, viruses are very good at targeting specific cells. In gene therapy, viral vectors are changed so they do not create a new virus in the cell, but just drop off a new gene.

Many scientists are searching for ‘suicide genes’ that would attack cancer cells, while leaving normal cells untouched. Gene therapy is a fairly new treatment approach, still very much in the experimental stages, and cannot be administered without the patient’s participation in a clinical trial.
Immunotherapy
Immunotherapy is also known as biological therapy, biotherapy, or biological response modifier (BRM) therapy. It is a treatment designed to stimulate the body’s own natural immune defenses to stop the spread of cancer. Scientists have determined that the immune system can recognize and eliminate cancer cells under some circumstances. The problem with mesothelioma is that the body does not recognize the cancer cells as abnormal.
Immunotherapy uses BRMs to boost the body’s natural ability to fight disease. Interferons, interleukins, tumor necrosis factors, monoclonal antibodies and cancer vaccines are all BRMs. Some occur naturally in the body, and others are generated synthetically in the lab. BRMs seem to change the body’s relationship with mesothelioma cells, so the body recognizes them as abnormal. As a result, the body’s ‘immune response’ kicks in to attack the mesothelioma cells and prevent the cancer from growing. Immunotherapy also seeks to block the process by which mesothelioma alters a normal cell into a cancer cell. Scientists hope that BRMs can stop the migration of mesothelioma to other parts of the body, and prevent its further growth.
Preliminary studies have demonstrated considerable shrinkage of tumors at very early stages of mesothelioma. But more research is required to determine whether immunotherapy will be effective as a mesothelioma treatment. In Phase I and Phase II clinical trials of a combined immunotherapeutic and chemotherapeutic approach for mesothelioma patients, the results failed to show any meaningful effect on survival or relapse rate.
Photodynamic Therapy
Photodynamic therapy (PDT) uses a drug that is activated by light and applies laser light to it. The two work together to target and destroy cancer cells while keeping damage to surrounding healthy tissue at a minimum. The therapy begins with the patient’s injection with a non-toxic photosensitizer drug. The drug invades all cells of the body, but in about two days, normal cells excrete the drug. Then the patient is exposed to laser light, which will activate the drug remaining in the cancer cells and destroy them. Timing is critical, because the tumor cells must be exposed to the laser light after the drug is excreted by the normal cells, but before the drug is expelled by the mesothelioma cells.
It is unclear what role photodynamic therapy may play in the treatment of mesothelioma. Since the laser light cannot be absorbed at any great depth in the body, treatment via PDT can only be used on superficial areas of the body. Still, the treatment may be ideal for the treatment of mesothelioma after surgical removal of the tumor. Some doctors have applied PDT intraoperatively after surgery, but the number of patients treated in clinical trials is small, making it difficult to draw definitive conclusions. Most reports concerning PDT are Phase I and II studies and the only phase III study was conducted with an earlier generation photosensitizer. That study reported no advantage in using PDT in combination with surgery and immunochemotherapy. At present, all that is known is that PDT can be performed safely with newer generation photosensitizers and that results are encouraging for mesothelioma patients with stages I and II disease.